This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through a series of inputs from an available global online community of experts with an aim to solve those patient's clinical problems with collective,current,best evidence based inputs.
This e-log book also reflects my patient centered online learning portfolio and your valuable inputs in the comment box is welcome. Case:
A 28 year male who is electrician and a resident of Nalgonda was admitted to hospital on 25/05/2021 with chief complaints of
- Fever since 4 days
-Cough since 2 days
-Pain in epigastrium since morning
History of present illness:
The patient was apparently asymptomatic 4 days ago then he developed
- Fever which was insidious in onset, intermittent in nature ,high grade and associated with chills and rigor
-cough was since 2 days , which was productive ,white coloured sputum and occasionally blood tinged
-pain in epigastrium since morning which is dragging type ,non - radiating and associated with cough
-Not associated with peadal odema , vomiting,loose stool ,shortness of breath
-RT-PCR test for corona virus is positive.
History of past illness:
The patient is not a known case of diabetes , hypertension,asthma, epilepsy.
Family history :
Insignificant
No COVID contacts
Personal history:
Appetite -Normal
Diet- Mixed
Bowel and bladder habits - Regular
Sleep- Adequate
Addictions-Occasionally alcoholic
General examination:
Patient was examined in a well lit room, after informed consent.
He was conscious, coherent and cooperative. Moderately built and nourished.
No pallor, icterus, cyanosis,clubbing,koilonychia,lymphadenopathy or generalized edema were observed
Vitals:
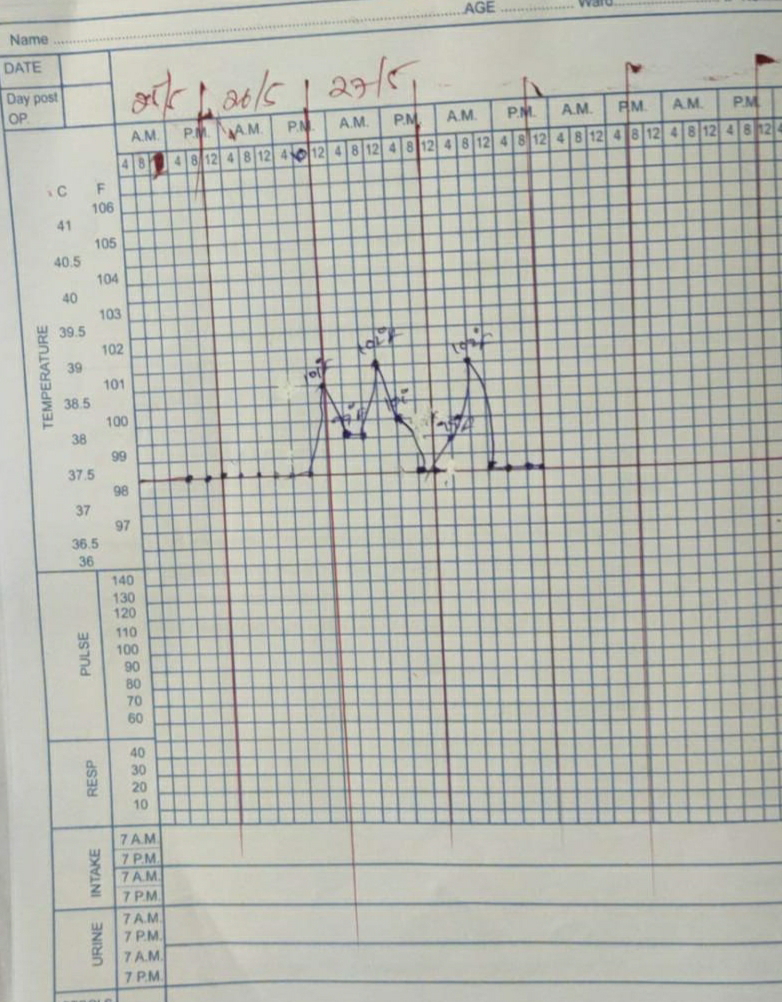
On 25/05/21:
Temperature:98.6F
PR:74/min
BP:120/70 mm Hg
RR:24/min
On 26/05/21:
Temperature:100F
PR:120/min
BP:120/80mm Hg
RR:21/min
On 27/05/21:
Temperature:99.2F
PR:98/min
BP:110/80 mm Hg
RR:120/min
Systemic examination:
CVS:S1,S2 heart sounds,no murmers
Respiratory system :Bilateral air entry present
CNS :Intact
Abdomen:Softand nontender,no organomegaly Vitals:Invetigations:C REACTIVE PROTEIN:
Interpretation:LFT:
AST:44IU/L(Increased)
ALT:64IU/L(Increased)
Alkaline phosphatase:141IU/L (Increased)
RFT:
Creatinine:0.7 mg/dl
Uric acid:3mg/dl(Decreased)
ECG:
HRCT images:
Provisional diagnosis:Mild pneumonia secondary to COVID-19
Treatment:
On 25/05/21,26/05/21,27/05/21
-O2 inhalation if spO2 is less than 92%
-Tab.PAN 40 mg OD
-Tab.PCM 650 mg TID
-Inj NEOMOL 1 gm IV
-Tab LiMCEE 50 mg OD
-Tab MVT OD
- syp Ascoryl 10 ml TID
-Inj.ENOXAPARAN 40 mg
- Nebulization with DUOLIN and BUDECORT
-Inj.DEXA 8mg/IV/ OD
-Inj.AUGMENTIN 1.2gm/IV/BD
-Tab.Ultracet 1/2 tab BD
28/05/21:
Vitals:
Temperature:102F
PR:82/min
BP:120/80mm Hg
RR:26/min
SpO2:94%
D-Dimer:370mg/dl
Fever chart:
WBC count: 24/05:9800cells/mm3
27/05:15,800cells/mm3
28/05:23,500cells/mm3
Treatment:
O2 inhalation if spO2 is less than 92%
-Tab.PAN 40 mg OD
-Tab.PCM 650 mg TID
-Inj NEOMOL 1 gm IV
-Tab LiMCEE 50 mg OD
-Tab MVT OD
- syp Ascoryl 10 ml TID
-Inj.ENOXAPARAN 40 mg
- Nebulization with DUOLIN and BUDECORT
-Inj.DEXA 8mg/IV/ OD
-Inj.AUGMENTIN 1.2gm/IV/BD
-Tab.Ultracet 1/2 tab BD
-Spirometry,prone positioning
I would like thank Dr.Rakesh Biswas sir for the opportunity and Dr.Sai Charan sir for your guidance.