50yr male with pyrexia
Case:
50 male came with chief complaints of
-Fever from 4 days
- Loose motions from 3 days
HOPI:
Patient was apparently asymptomatic 4 days back then he developed fever which is high grade, intermitent, relieved on medication
-Loose stools from 3 days , insidious in onset ,blackish discoloration, liquid in consistency
-vomiting one episode yesterday,non-bilious,no blood,non-projectile,food as content
- SOB Grade 3 from 1 days
Past History:
K/C/O DM since 5 months ,not on regular medication
N/K/C/O HTN,TB,Asthma,CVA,CAD
H/O Fracture of femur 10 years ago
Personal History:
Appetite: Reduced
Diet:Mixed
Sleep: Adequate
Bowel and bladder habits: Loose motions
General Examination:
Patient is conscious, coherent, co-operative
Well oriented to time, place and person
Moderately built and nourished
No pallor, icterus, cyanosis, clubbing, pedal oedema, lymphadenopathy
PR:104 bpm
BP:110/70 mm Hg
Temp:98.1F
RR:22cpm
CVS:S1S2 Present
RS:
Inspection:
Shape of chest: Elliptical
Trachea- Central
No scars,sinuses, engorged veins
Palpation:
Trachea- Central
Apex beat felt at 5 th ICS
Auscultation:
Creptations present at right IAA,IMA and left IAA
Abdominal Examination:
Inspection:
Shape of abdomen: Scaphoid
All quadrants moving equally with respiration
No scars,sinuses, engorged veins
Palpation:
Tenderness in right hypochondrium, epigastrium,left hypochondrium
No shifting dullness
Auscultation: Bowel sounds present
CNS:NAD
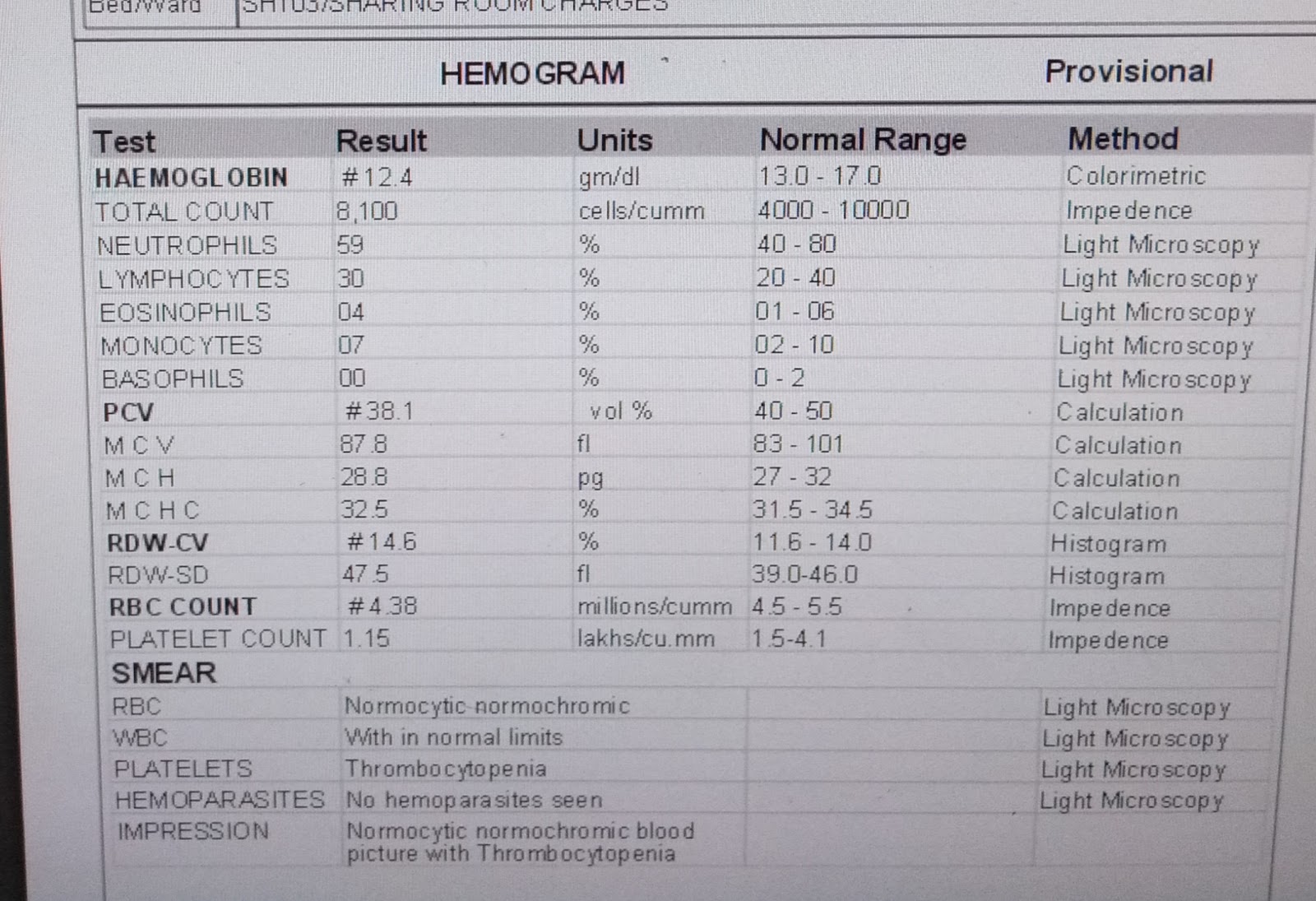
Investigations:
Provisional Diagnosis: Pyrexia under evaluation with thrombocytopenia
With DM
Treatment:
1)IV fluids NS ,RL @ 100ml/hr
2)T.DOXY100MG PO/BD
3)T.PAN 40 MG PO/OD
4)T.ZOFER 4 MG PO/SOS
5)T.PCM 650 MG PO/SOS
DEATH SUMMARY:
50 yr old male patient came with c/o fever since 4 days,high grade, vomiting ,loose stools:4 days,sob -1 day,k/c/o DM : 5 months with vitals at presentation BP:100/60 mm hg ,PR:104 bpm,SPo2:90 at RA ,RR: 28 cpm,B/L basal crepts was provisionallly diagnosed as ?viral pyrexia with severe thrombocytopenia 6000 with bleeding manifestations -Malena,haematuria with acute lung injury,MODS,Sepsis.Patient was started on SDP transfusion 2 units ,emperical antibiotics,IV fluids,Diuretics, intermittent NIV, Oxygen.On day 2 of admission patient has worsening tachpnea, worsening x ray changes progressed to ARDS, Platelet count 19,000 with Malena .3 rd SDP transfusion was done on day 2 of admission.Consent was not given for elective intubation and mechanical ventilation .Treated with intermittent NIV, Antibiotics were escalated . patient has worsening tachpnea falling spo2 on day 4 of admission followed by profuse sweating and cardiac arrest at 7:15 am .CPR was initiated immediately,8 cycles was done.Inspite of all above efforts patient could not be raised and declared dead at 7:55 am as ECG showed flat line
Immediate cause of death: Type 1 respiratory failure,acte respiratory distress syndrome
Antecedent cause of DEATH: SEPSIS with MODS,Acute lung injury, Acute kidney injury,Acute liver injury
Comorbidities: Diabetes mellitus since 5 months